Augmentation Mammaplasty (Breast Enlargement)

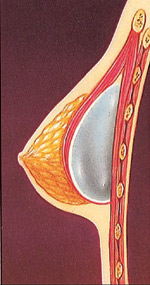
Breast Implant
Breast augmentation is one of the commonest procedures performed at plastic surgicentre in Doha, Qatar. Breast augmentation, technically known as augmentation mammoplasty, is a surgical procedure to enhance the size and shape of a woman’s breast for a number of reasons:
To enhance the body contour of a woman who, for personal reasons, feels her breast size is too small.
To correct a reduction in breast volume after pregnancy.
To balance a difference in breast size.
As a reconstructive technique following breast surgery.
By inserting an implant behind each breast, surgeons are able to increase a woman’s bust line by one or more bra cup sizes. If you’re considering breast augmentation, the following information will give you a basic understanding of the procedure – when it can help, how it’s performed, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please ask your surgeon if there is anything you don’t understand about the procedure.
Breast augmentation is usually done to balance a difference in breast size, to improve body
Breast augmentation is usually done to balance a difference in breast size, to improve body contour, or as a reconstructive technique following surgery.
contour, or as a reconstructive technique following surgery.
The best candidates for breast augmentation
Breast augmentation can enhance your appearance and your self-confidence, but it won’t necessarily change your looks to match your ideal, or cause other people to treat you differently. Before you decide to have surgery, think carefully about your expectations and discuss them with your surgeon.
The best candidates for breast augmentation are women who are looking for improvement, not perfection, in the way they look. If you’re physically healthy and realistic in your expectations, you may be a good candidate.
Types of implants
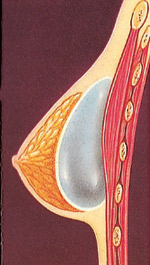
A breast implant is a silicone shell filled with either silicone gel or a salt-water solution known as saline.
All surgery carries some uncertainty and risk
Breast augmentation is relatively straightforward. But as with any operation, there are risks associated with surgery and specific complications associated with this procedure.
The most common problem, capsular contracture, occurs if the scar or capsule around the implant begins to tighten. This squeezing of the soft implant can cause the breast to feel hard. Capsular contracture can be treated in several ways, and sometimes requires either removal or “scoring” of the scar tissue, or perhaps removal or replacement of the implant.
As with any surgical procedure, excessive bleeding following the operation may cause some swelling and pain. If excessive bleeding continues, another operation may be needed to control the bleeding and remove the accumulated blood.
A small percentage of women develop an infection around an implant. This may occur at any time, but is most often seen within a week after surgery. In some cases, the implant may need to be removed for several months until the infection clears. A new implant can then be inserted. Some women report that their nipples become oversensitive, under sensitive, or even numb. You may also notice small patches of numbness near your incisions. These symptoms usually disappear with time, but may be permanent in some patients.
There is no evidence that breast implants will affect fertility, pregnancy, or your ability to nurse. If, however, you have nursed a baby within the year before augmentation, you may produce milk for a few days after surgery. This may cause some discomfort.
Occasionally, breast implants may leak. Rupture can occur as a result of injury, causing the man-made shell to leak. If a saline filled implant breaks, the implant will deflate in a few hours and the salt water will be harmlessly absorbed by the body.
If a break occurs in a gel-filled implant, however, one of two things may occur. If the shell breaks but the scar capsule around the implant does not, you may not detect any change. If the scar also breaks or tears, especially following extreme pressure, silicone gel may move into surrounding tissue. The gel may collect in the breast and cause a new scar to form around it. There may be a change in the shape or firmness of the breast. Both types of breaks may require a second operation and replacement of the leaking implant.
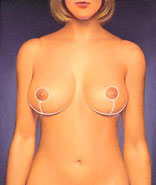
After surgery, breasts appear fuller and more natural in tone and contour. Scars will fade with time.
A few women with breast implants have reported symptoms similar to scleroderma and other arthritis-like conditions. These symptoms may include joint pain or swelling, or breast pain. Research has found no link between silicone breast implants and these symptoms .
While there is no evidence that breast implants cause breast cancer, they may change the way mammography is done to detect cancer. When you request a routine mammogram, be sure to go to a radiology center where technicians are experienced in the special techniques required to get a reliable x-ray of a breast with an implant. Additional views will be required. Ultrasound examinations may be of benefit in some women with implants to detect breast lumps or to evaluate the implant.
While the majority of women do not experience these complications, you should discuss each of them with your physician to make sure you understand the risks and consequences of breast augmentation.
After surgery, breasts appear fuller and more natural in tone and contour. Scars will fade with time.
Planning your surgery
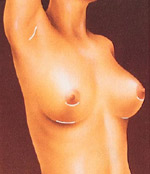
After surgery, breasts appear fuller and more natural in tone and contour. Scars will fade with time.
In your initial consultation, Dr. Makki will evaluate your health and explain which surgical techniques are most appropriate for you, based on the condition of your breasts and skin tone. If your breasts are sagging, Dr. Makki may also recommend a breast lift.
Be sure to discuss your expectations frankly with Dr. Makki. He will be equally frank with you, describing your alternatives and the risks and limitations of each. And, be sure to tell Dr. Makki if you smoke, and if you’re taking any medications, vitamins, or other drugs.
Dr. Makki will also explain the type of anesthesia to be used, the type of facility where the surgery will be performed, and the costs involved. Because most insurance companies do not consider breast augmentation to be medically necessary, carriers generally do not cover the cost of this procedure.
Preparing for your surgery
Dr. Makki will give you instructions to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications.
While making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days, if needed.
Where your surgery will be performed
Your surgery may be prefer performed in an office facility, a freestanding surgery center, or a hospital outpatient facility. Occasionally, the surgery may be done as an inpatient in a hospital, in which case you can plan on staying for a day or two.
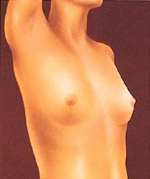
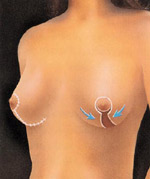
Incisions are made to keep scars as inconspicuous as possible, in the breast crease, around the nipple, or in the armpit.
Types of anesthesia
Incisions are made to keep scars as inconspicuous as possible, in the breast crease, around the nipple, or in the armpit.
Breast augmentation can be performed with a general anesthesia, so you’ll sleep through the entire operation. Some surgeons may use a local anesthesia, combined with a sedative to make you
Incisions are made to keep scars as inconspicuous as possible, in the breast crease, around the nipple, or in the armpit.
drowsy, so you’ll be relaxed but awake, and may feel some discomfort.
The surgery
The method of inserting and positioning your implant will depend on your anatomy and your surgeon’s recommendation. The incision can be made either in the crease where the breast meets the chest, around the areola (the dark skin surrounding the nipple), or in the armpit. Every effort will be made to assure that the incision is placed so resulting scars will be as inconspicuous as possible.
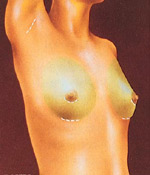
Working through the incision, the surgeon will lift your breast tissue and skin to create a pocket, either directly behind the breast tissue or underneath your chest wall muscle (the pectoral muscle). The implants are then centered beneath your nipples.
The breast implant may be inserted directly under breast tissue.
Some surgeons believe that putting the implants behind your chest muscle may reduce the potential for capsular contracture. This placement may also interfere less with breast examination by mammogram than if the implant is placed directly behind the breast tissue. Placement behind the muscle however, may be more painful for a few days after surgery than placement directly under the breast tissue. Drainage tubes may be used for several days following the surgery.
You’ll want to discuss the pros and cons of these alternatives with Dr. Makki before surgery to make sure you fully understand the implications of the procedure he recommends for you. The surgery usually takes one to two hours to complete. Stitches are used to close the incisions, which may also be taped for greater support. A gauze bandage may be applied over your breasts to help with healing.
The breast implant may be inserted directly under breast tissue.
After your surgery
The breast implant may be inserted directly under breast tissue.
The breast implant may be inserted directly under the chest wall muscle.
You’re likely to feel tired and sore for a few days following your surgery, but you’ll be up and around in 24 to 48 hours. Most of your discomfort can be controlled by medication prescribed by Dr. Makki.
Within several days, the gauze dressings, if you have them, will be removed, and you may be given a surgical bra. You may also experience a burning sensation in your nipples for about two weeks, but this will subside as bruising fades.
Your stitches will dissolve over time, but the swelling in your breasts may take three to five weeks to disappear.
The breast implant may be inserted directly under the chest wall muscle.
The breast implant may be inserted directly under the chest wall muscle.
Getting back to normal
You should be able to return to work within a few days, depending on the level of activity required for your job.
Follow Dr. Makki’s advice on when to begin exercises and normal activities. Your breasts will probably be sensitive to direct stimulation for two to three weeks, so you should avoid much physical contact. After that, breast contact is fine once your breasts are no longer sore, usually three to four weeks after surgery.
Your scars will be firm and pink for at least six weeks. Then they may remain the same size for several months, or even appear to widen. After several months, your scars will begin to fade, although they will never disappear completely.
Routine mammograms should be continued after breast augmentation for women who are in the appropriate age group, although the mammographic technician should use a special technique to assure that you get a reliable reading, as discussed earlier.
Your new look

For many women, the result of breast augmentation can be satisfying, even exhilarating, as they learn to appreciate their fuller appearance.
For many women, the result of breast augmentation can be satisfying, even exhilarating, as they learn to appreciate their fuller appearance.
Your decision to have breast augmentation is a highly personal one that not everyone will understand. The important thing is how you feel about it. If you’ve met your goals, then your surgery is a success.
The information on this web site is only intended as an introduction to this procedure and should not be used to determine whether you will have the procedure performed nor as a guarantee of the result.
The best method of determining your personal options is to schedule a personal consultation with Dr. Makki. He will be able to answer specific questions related to your situation.
Please don’t hesitate to call for any questions that you might have
Mastopexy (Breast Lift)
Breast lift is commonly performed at plastic surgicentre in Doha, Qatar.
Over the years, factors such as pregnancy, nursing, and the force of gravity take their toll on a woman’s breasts. As the skin loses its elasticity, the breasts often lose their shape and firmness and begin to sag. Breast lift, or mastopexy, is a surgical procedure to raise and reshape sagging breasts – at least, for a time. (No surgery can permanently delay the effects of gravity.) Mastopexy can also reduce the size of the areola, the darker skin surrounding the nipple. If your breasts are small or have lost volume – for example, after pregnancy-breast implants inserted in conjunction with mastopexy can increase both their firmness and their size. If you’re considering a breast lift, the following information will give you a basic understanding of the procedure – when it can help, how it’s performed, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please be sure to ask your doctor if there is any thing about the procedure you don’t understand.

Over time, a woman’s breasts begin to sag and the areolas become larger.
Over time, a woman’s breasts begin to sag and the areolas become larger.
The best candidates for breast lift
A breast lift can enhance your appearance and your self-confidence, but it won’t necessarily change your looks to match your ideal, or cause other people to treat you differently. Before you decide to have surgery, think carefully about your expectations and discuss them with your surgeon.
The best candidates for mastopexy are healthy, emotionally stable women who are realistic about what the surgery can accomplish. The best results are usually achieved in women with small, sagging breasts. Breasts of any size can be lifted, but the results may not last as long in heavy breasts.
Many women seek mastopexy because pregnancy and nursing have left them with stretched skin and less volume in their breasts. However, if you’re planning to have more children, it may be a good idea to postpone your breast lift. While there are no special risks that affect future pregnancies (for example, mastopexy usually doesn’t interfere with breast-feeding), pregnancy is likely to stretch your breasts again and offset the results of the procedure.
All surgery carries some uncertainty and risk
A breast lift is not a simple operation, but it’s normally safe when performed by a qualified plastic surgeon. Nevertheless, as with any surgery, there is always a possibility of complications or a reaction to the anesthesia. Bleeding and infection following a breast lift are uncommon, but they can cause scars to widen. You can reduce your risks by closely following your physician’s advice both before and after surgery.
Mastopexy does leave noticeable, permanent scars, although they’ll be covered by your bra or bathing suit. (Poor healing and wider scars are more common in smokers.) The procedure can also leave you with unevenly positioned nipples, or a permanent loss of feeling in your nipples or breasts.
Planning your surgery
In your initial consultation, it’s important to discuss your expectations frankly with your surgeon, and to listen to his or her opinion. Every patient – and every physician, as well – has a different view of what is a desirable size and shape for breasts.
The surgeon will examine your breasts and measure them while you’re sitting or standing. He or she will discuss the variables that may affect the procedure-such as your age, the size and shape of your breasts, and the condition of your skin-and whether an implant is advisable. You should also discuss where the nipple and areola will be positioned; they’ll be moved higher during the procedure, and should be approximately even with the crease beneath your breast.
Your surgeon should describe the procedure in detail, explaining its risks and limitations and making sure you understand the scarring that will result. He or she should also explain the anesthesia to be used, the type of facility where the surgery will be performed, and the costs involved.
Don’t hesitate to ask your doctor any questions you may have, especially those regarding your expectations and concerns about the results.
Preparing for your surgery
Depending on your age and family history, your surgeon may require you to have a mammogram (breast x-ray) before surgery. You’ll also get specific instructions on how to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications.
While you’re making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days if needed.
Where your surgery will be performed
Your breast lift may be performed in a hospital, an outpatient surgery center, or a surgeon’s office-based facility. It’s usually done on an outpatient basis, for cost containment and convenience. If you’re admitted to the hospital as an inpatient, you can expect to stay one or two days.
Types of anesthesia
Breast lifts are usually performed under general anesthesia, which means you’ll sleep through the operation.
In selected patients – particularly when a smaller incision is being made – the surgeon may use local anesthesia, combined with a sedative to make you drowsy. You’ll be awake but relaxed, and will feel minimal discomfort.
The surgery
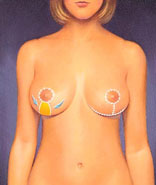
Mastopexy usually takes one and a half to three and a half hours. Techniques vary, but the most common procedure involves an anchor-shaped incision following the natural contour of the breast.
The incision outlines the area from which breast skin will be removed and defines the new location for the nipple. When the excess skin has been removed, the nipple and areola are moved to the higher position. The skin surrounding the areola is then brought down and together to reshape the breast. Stitches are usually located around the areola, and in a vertical line extending downwards from the nipple area.
Skin formerly located above the nipple is brought down and together to reshape the breast. Sutures close the incisions, giving the breast it’s new contour.
Some patients, especially those with relatively small breasts and minimal sagging, may be candidates for modified procedures requiring less extensive incisions. One such procedure is the “doughnut (or concentric) mastopexy,” in which circular incisions are made around the areola, and a doughnut-shaped area of skin is removed.
If you’re having an implant inserted along with your breast lift, it will be placed in a pocket directly under the breast tissue, or deeper, under the muscle of the chest wall.
Skin formerly located above the nipple is brought down and together to reshape the breast. Sutures close the incisions, giving the breast it’s new contour
Skin formerly located above the nipple is brought down and together to reshape the breast. Sutures close the incisions, giving the breast it’s new contour
After your surgery
After surgery, you’ll wear an elastic bandage or a surgical bra over gauze dressings. Your breasts will be bruised, swollen, and uncomfortable for a day or two, but the pain shouldn’t be severe. Any discomfort you do feel can be relieved with medications prescribed by your surgeon.
Within a few days, the bandages or surgical bra will be replaced by a soft support bra. You’ll need to wear this bra around the clock for three to four weeks, over a layer of gauze. The stitches will be removed after a week or two.
If your breast skin is very dry following surgery, you can apply a moisturizer several times a day. Be careful not to tug at your skin in the process, and keep the moisturizer away from the suture areas. You can expect some loss of feeling in your nipples and breast skin, caused by the swelling after surgery. This numbness usually fades as the swelling subsides over the next six weeks or so. In some patients, however, it may last a year or more, and occasionally it may be permanent.
Getting back to normal
Healing is a gradual process. Although you may be up and about in a day or two, don’t plan on returning to work for a week or more, depending on how you feel. And avoid lifting anything over your head for three to four weeks. If you have any unusual symptoms, don’t hesitate to call your surgeon.
Your surgeon will give you detailed instructions for resuming your normal activities. You may be instructed to avoid sex for a week or more, and to avoid strenuous sports for about a month. After that, you can resume these activities slowly. If you become pregnant, the operation should not affect your ability to breast-feed, since your milk ducts and nipples will be left intact.
Your new look

Long lasting results
Your surgeon will make every effort to make your scars as inconspicuous as possible. Still, it’s important to remember that mastopexy scars are extensive and permanent. They often remain lumpy and red for months, then gradually become less obvious, sometimes eventually fading to thin white lines. Fortunately, the scars can usually be placed so that you can wear even low-cut tops.
You should also keep in mind that a breast lift won’t keep you firm forever-the effects of gravity, pregnancy, aging, and weight fluctuations will eventually take their toll again. Women who have implants along with their breast lift may find the results last longer.
Your satisfaction with a breast lift is likely to be greater if you understand the procedure thoroughly and if your expectations are realistic.
The information on this web site is only intended as an introduction to this procedure and should not be used to determine whether you will have the procedure performed nor as a guarantee of the result.
The best method of determining your personal options is to schedule a personal consultation with Dr. Makki. He will be able to answer specific questions related to your situation.
Please don’t hesitate to call for any questions that you might have
Reduction Mammaplasty (Breast Reduction)

Heavy breasts can lead to physical discomfort, a variety of medical problems, shoulder indentations due to tight bra straps, and extreme self-consciousness.
Heavy breasts can lead to physical discomfort, a variety of medical problems, shoulder indentations due to tight bra straps, and extreme self-consciousness.
Breast reduction is commonly performed at plastic surgicentre in Doha, Qatar.
IF YOU ARE CONSIDERING BREAST REDUCTION
Women with very large, pendulous breasts may experience a variety of medical problems caused by the excessive weight-from back and neck pain and skin irritation to skeletal deformities and breathing problems. Bra straps may leave indentations in their shoulders. And unusually large breasts can make a woman-or a teenage girl-feel extremely self-conscious.
Breast reduction, technically known as reduction mammaplasty, is designed for such women. The procedure removes fat, glandular tissue, and skin from the breasts, making them smaller, lighter, and firmer. It can also reduce the size of the areola, the darker skin surrounding the nipple. The goal is to give the woman smaller, better-shaped breasts in proportion with the rest of her body.
If you’re considering breast reduction, this will give you a basic understanding of the procedure- when it can help, how it’s performed, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please be sure to ask doctor Makki if there is anything about the procedure you don’t understand.
THE BEST CANDIDATE FOR BREAST REDUCTION
Breast reduction is usually performed for physical relief rather than simply cosmetic improvement. Most women who have the surgery are troubled by very large, sagging breasts that restrict their activities and cause them physical discomfort.
In most cases, breast reduction isn’t performed until a woman’s breasts are fully developed; however, it can be done earlier if large breasts are causing serious physical discomfort. The best candidates are those who are mature enough to fully understand the procedure and have realistic expectations about the results. Breast reduction is not recommended for women who intend to breast-feed.
ALL SURGERY CARRIES SOME UNCERTAINTY AND RISK
Breast reduction is not a simple operation, but it’s normally safe when performed by a qualified plastic surgeon. Nevertheless, as with any surgery, there is always a possibility of complications, including bleeding, infection, or reaction to the anesthesia. Some patients develop small sores around their nipples after surgery; these can be treated with antibiotic creams. You can reduce your risks by closely following Dr Makki’s advice both before and after surgery.
The procedure does leave noticeable, permanent scars, although they’ll be covered by your bra or bathing suit. (Poor healing and wider scars are more common in smokers.) The procedure can also leave you with slightly mismatched breasts or unevenly positioned nipples. Future breast-feeding may not be possible, since the surgery removes many of the milk ducts leading to the nipples.
Some patients may experience a permanent loss of feeling in their nipples or breasts. Rarely, the nipple and areola may lose their blood supply and the tissue will die. (The nipple and areola can usually be rebuilt, however, using skin grafts from elsewhere on the body.)
PLANNING YOUR SURGERY
In your initial consultation, it’s important to discuss your expectations frankly with Dr Makki, and to listen to his opinion. Every patient-and every physician, as well-has a different view of what is a desirable size and shape for breasts.
Dr Makki will examine and measure your breasts, and will probably photograph them for reference during surgery and afterwards. (The photographs may also be used in the processing of your insurance coverage.) He will discuss the variables that may affect the procedure-such as your age, the size and shape of your breasts, and the condition of your skin. You should also discuss where the nipple and areola will be positioned; they’ll be moved higher during the procedure, and should be approximately even with the crease beneath your breasts.
Dr Makki should describe the procedure in detail, explaining its risks and limitations and making sure you understand the scarring that will result. Dr Makki should also explain the anesthesia he will use, the facility where the surgery will be performed, and the costs. (Some insurance companies will pay for breast reduction if it’s medically necessary; however, they may require that a certain amount of breast tissue be removed. Check your policy.)
PREPARING FOR YOUR SURGERY
Dr Makki may require you to have a mammogram (breast x-ray) before surgery. You’ll also get specific instructions on how to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications.
Breast reduction doesn’t usually require a blood transfusion. However, if a large amount of breast tissue will be removed, Dr Makki may advise you to have a unit of blood drawn ahead of time. That way, if a transfusion should be needed, your own blood can be used.
While you’re making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days if needed.
WHERE YOUR SURGERY WILL BE PERFORMED
Breast reduction surgery may be performed in a hospital, an outpatient surgery center or an office-based surgical suite. If you are admitted to the hospital, your stay will be a short one. The surgery itself usually takes two to four hours, but may take longer in some cases.
TYPE OF ANESTHESIA
Breast reduction is nearly always performed under general anesthesia. You’ll be asleep through the entire operation.
Incisions outline the area of skin, breast tissue, and fat to be removed and the new position for the nipple.

Incisions outline the area of skin, breast tissue, and fat to be removed and the new position for the nipple.
THE SURGERY
Techniques for breast reduction vary, but the most common procedure involves an anchor-shaped incision that circles the areola, extends downward, and follows the natural curve of the crease beneath the breast. The surgeon removes excess glandular tissue, fat, and skin, and moves the nipple and areola into their new position. He then brings the skin from both sides of the breast down and around the areola, shaping the new contour of the breast. Liposuction may be used to remove excess fat from the armpit area.
In most cases, the nipples remain attached to their blood vessels and nerves. However, if the breasts are very large or pendulous, the nipples and areolas may have to be completely removed and grafted into a higher position. (This will result in a loss of sensation in the nipple and areolar tissue.)
Skin formerly located above the nipple is brought down and together to reshape the breast. Sutures close the incisions, giving the breast it’s new contour.
Stitches are usually located around the areola, in a vertical line extending downward, and along the lower crease of the breast. In some cases, techniques can be used that eliminate the vertical part of the scar. And occasionally, when only fat needs to be removed, liposuction alone can be used to reduce breast size, leaving minimal scars.
Skin formerly located above the nipple is brought down and together to reshape the breast. Sutures close the incisions, giving the breast it’s new contour.
Scars around the areola, below it, and in the crease under the breast are permanent, but can be easily concealed by clothing.
AFTER YOUR SURGERY
After surgery, you’ll be wrapped in an elastic bandage or a surgical bra over gauze dressings. A small tube may be placed in each breast to drain off blood and fluids for the first day or two.
You may feel some pain for the first couple of days-especially when you move around or cough-and some discomfort for a week or more. Dr Makki will prescribe medication to lessen the pain.
The bandages will be removed a day or two after surgery, though you’ll continue wearing the surgical bra around the clock for several weeks, until the swelling and bruising subside. Your stitches will be removed in one to three weeks.
If your breast skin is very dry following surgery, you can apply a moisturizer several times a day, but be sure to keep the suture area dry.
Scars around the areola, below it, and in the crease under the breast are permanent, but can be easily concealed by clothing.
Your first menstruation following surgery may cause your breasts to swell and hurt. You may also experience random, shooting pains for a few months. You can expect some loss of feeling in your nipples and breast skin, caused by the swelling after surgery. This usually fades over the next six weeks or so. In some patients, however, it may last a year or more, and occasionally it may be permanent.
GETTING BACK TO NORMAL
Although you may be up and about in a day or two, your breasts may still ache occasionally for a couple of weeks. You should avoid lifting or pushing anything heavy for three or four weeks.
Dr Makki will give you detailed instructions for resuming your normal activities. Most women can return to work (if it’s not too strenuous) and social activities in about two weeks. But you’ll have much less stamina for several weeks, and should limit your exercises to stretching, bending, and swimming until your energy level returns. You’ll also need a good athletic bra for support.
You may be instructed to avoid sex for a week or more, since sexual arousal can cause your incisions to swell, and to avoid anything but gentle contact with your breasts for about six weeks.
A small amount of fluid draining from your surgical wound, or some crusting, is normal. If you have any unusual symptoms, such as bleeding or severe pain, don’t hesitate to call your doctor.
With smaller, better proportioned breasts, you’ll feel more comfortable and your clothes will fit better.
With smaller, better proportioned breasts, you’ll feel more comfortable and your clothes will fit better.
YOUR NEW LOOK
Although much of the swelling and bruising will disappear in the first few weeks, it may be six months to a year before your breasts settle into their new shape. Even then, their shape may fluctuate in response to your hormonal shifts, weight changes, and pregnancy.
Dr Makki will make every effort to make your scars as inconspicuous as possible. Still, it’s important to remember that breast reduction scars are extensive and permanent. They often remain lumpy and red for months, then gradually become less obvious, sometimes eventually fading to thin white lines. Fortunately, the scars can usually be placed so that you can wear even low-cut tops.
Of all plastic surgery procedures, breast reduction results in the quickest body-image changes. You’ll be rid of the physical discomfort of large breasts, your body will look better proportioned, and clothes will fit you better.
However, as much as you may have desired these changes, you’ll need time to adjust to your new image-as will your family and friends. Be patient with yourself, and with them. Keep in mind why you had this surgery, and chances are that, like most women, you’ll be pleased with the results.
The information on this web site is only intended as an introduction to this procedure and should not be used to determine whether you will have the procedure performed nor as a guarantee of the result.
The best method of determining your personal options is to schedule a personal consultation with Dr. Makki. He will be able to answer specific questions related to your situation.
Please don’t hesitate to call for any questions that you might have
Gynecomastia (Breast reduction for men )
Gynecomastia
Gynecomastia is a medical term that comes from the Greek words for “women-like breasts.” Though this oddly named condition is rarely talked about, it’s actually quite common. It is commonly seen at plastic surgicentre in Doha, Qatar. Gynecomastia affects an estimated 40 to 60 percent of men. It may affect only one breast or both. Though certain drugs and medical problems have been linked with male breast overdevelopment, there is no known cause in the vast majority of cases.
For men who feel self-conscious about their appearance, breast-reduction surgery can help. The procedure removes fat and or glandular tissue from the breasts, and in extreme cases removes excess skin, resulting in a chest that is flatter, firmer, and better contoured.
If you’re considering surgery to correct gynecomastia, this information will give you a basic understanding of the procedure–when it can help, how it’s performed, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please be sure to ask your doctor if there is anything about the procedure you don’t understand
Many men have gynecomastia — enlarged, female-like breasts–causes by excess glandular tissue or fat (or both).
Many men have gynecomastia — enlarged, female-like breasts–causes by excess glandular tissue or fat (or both).
THE BEST CANDIDATES FOR GYNECOMASTIA CORRECTION
Surgery to correct gynecomastia can be performed on healthy, emotionally stable men of any age. The best candidates for surgery have firm, elastic skin that will reshape to the body’s new contours.
Surgery may be discouraged for obese men, or for overweight men who have not first attempted to correct the problem with exercise or weight loss. Also, individuals who drink alcohol beverages in excess or smoke marijuana are usually not considered good candidates for surgery. These drugs, along with anabolic steroids, may cause gynecomastia. Therefore, patients are first directed to stop the use of these drugs to see if the breast fullness will diminish before surgery is considered an option.
ALL SURGERY CARRIES SOME UNCERTAINTY AND RISK
When male breast-reduction surgery is performed by a qualified plastic surgeon, complications are infrequent and usually minor. Nevertheless, as with any surgery, there are risks. These include infection, skin injury, excessive bleeding, adverse reaction to anesthesia, and excessive fluid loss or accumulation. The procedure may also result in noticeable scars, permanent pigment changes in the breast area, or slightly mismatched breasts or nipples. If asymmetry is significant, a second procedure may be performed to remove additional tissue.
The temporary effects of breast reduction include loss of breast sensation or numbness, which may last up to a year.
PLANNING YOUR SURGERY
The initial consultation with your surgeon is very important. Your surgeon will need a complete medical history, so check your own records ahead of time and be ready to provide this information. First, your surgeon will examine your breasts and check for causes of the gynecomastia, such as impaired liver function, use of estrogen-containing medications, or anabolic steroids. If a medical problem is the suspected cause, you’ll be referred to an appropriate specialist.
Your plastic surgeon may, in extreme cases, also recommend a mammogram, or breast x-ray. This will not only rule out the very small possibility of breast cancer, but will reveal the breast’s composition. Once your surgeon knows how much fat and glandular tissue is contained within the breasts, he or she can choose a surgical approach to best suit your needs.
Don’t hesitate to ask your surgeon any questions you may have during the initial consultation- including your concerns about the recommended treatment or the costs involved. Treatment of gynecomastia may be covered by medical insurance–but policies vary greatly. Check your policy or call your carrier to be sure. If you are covered, make certain you get written pre-authorization for the treatment recommended by your surgeon.
PREPARING FOR YOUR SURGERY
Your surgeon will give you specific instructions on how to prepare for surgery, including guidelines on eating, drinking, and taking certain vitamins and medications.
Smokers should plan to stop smoking for a minimum of one or two weeks before surgery and during recovery. Smoking decreases circulation and interferes with proper healing. Therefore, it is essential to follow all your surgeon’s instructions.
WHERE YOUR SURGERY WILL BE PERFORMED
Surgery for gynecomastia is most often performed as an outpatient procedure, but in extreme cases, or those where other medical conditions present cause for concern, an overnight hospital stay may be recommended. The surgery itself usually takes about an hour and a half to complete. However, more extensive procedures may take longer.
TYPE OF ANESTHESIA
Correction of enlarged male breasts may be performed under general, or in some cases, under local anesthesia plus sedation. You’ll be awake, but very relaxed and insensitive to pain. More extensive correction may be performed under general anesthesia, which allows the patient to sleep through the entire operation. Your surgeon will discuss which option is recommended for you, and why this is the option of choice.
THE SURGERY

Gynecomastia
If excess glandular tissue is the primary cause of the breast enlargement, it will be excised, or cut out, with a scalpel. The excision may be performed alone or in conjunction with liposuction. In a typical procedure, an incision is made in an inconspicuous location–either on the edge of the areola or in the under arm area. Working through the incision, the surgeon cuts away the excess glandular tissue, fat and skin from around the areola and from the sides and bottom of the breast. Major reductions that involve the removal of a significant amount of tissue and skin may require larger incisions that result in more conspicuous scars. If liposuction is used to remove excess fat, the cannula is usually inserted through the existing incisions.
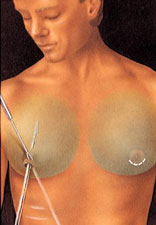
Gynecomastia
If your gynecomastia consists primarily of excessive fatty tissue, your surgeon will likely use liposuction to remove the excess fat. A small incision, less than a half-inch in length, is made around the edge of the areola–the dark skin that surrounds the nipple. Or, the incision may be placed in the underarm area. A slim hollow tube called a cannula which is attached to a vacuum pump, is then inserted into the incision. Using strong, deliberate strokes, the surgeon moves the cannula through the layers beneath the skin, breaking up the fat and suctioning it out. Patients may feel a vibration or some friction during the procedure, but generally no pain.
In extreme cases where large amounts of fat or glandular tissue have been removed, skin may not adjust well to the new smaller breast contour. In these cases, excess skin may have to be removed to allow the removing skin to firmly re-adjust to the new breast contour.
Sometimes, a small drain is inserted through a separate incision to draw off excess fluids. Once closed, the incisions are usually covered with a dressing. The chest may be wrapped to keep the skin firmly in place.
AFTER YOUR SURGERY
Whether you’ve had excision with a scalpel or liposuction, you will feel some discomfort for a few days after surgery. However, discomfort can be controlled with medications prescribed by your surgeon. In any case, you should arrange to have someone drive you home after surgery and to help you out for a day or two if needed.
You’ll be swollen and bruised for awhile–in fact, you may wonder if there’s been any improvement at all. To help reduce swelling, you’ll probably be instructed to wear an elastic pressure garment continuously for a week or two, and for a few weeks longer at night. Although the worst of your swelling will dissipate in the first few weeks, it may be three months or more before the final results of your surgery are apparent.
In the meantime, it is important to begin getting back to normal. You’ll be encouraged to begin walking around on the day of surgery, and can return to work when you feel well enough–which could be as early as a day or two after surgery. Any stitches will generally be removed about 1 to 2 weeks following the procedure.
Your surgeon may advise you to avoid sexual activity for a week or two, and heavy exercise for about three weeks. You’ll be told to stay away from any sport or job that risks a blow to the chest area for at least four weeks. In general, it will take about a month before you’re back to all of your normal activities.
You should also avoid exposing the resulting scars to the sun for at least six months. Sunlight can permanently affect the skin’s pigmentation, causing the scar to turn dark. If sun exposure is unavoidable, use a strong sunblock.
YOUR NEW LOOK
Your New Look
Gynecomastia surgery can enhance your appearance and self-confidence, but it won’t necessarily change your looks to match your ideal. Before you decide to have surgery, think carefully about your expectations and discuss them frankly with your plastic surgeon.
The results of the procedure are significant and permanent. If your expectations are realistic, chances are good that you’ll be very satisfied with your new look.
The information on this web site is only intended as an introduction to this procedure and should not be used to determine whether you will have the procedure performed nor as a guarantee of the result.
The best method of determining your personal options is to schedule a personal consultation with Dr. Makki. He will be able to answer specific questions related to your situation.
Please don’t hesitate to call for any questions that you might have
Breast Reconstruction

Breast Reconstruction
Facing the loss of one or both breasts can be very traumatic. Every women diagnosed with breast cancer should be given information about reconstructive options as part of her breast cancer treatment.
Almost any woman who loses her breast can have it rebuilt through reconstructive surgery. And discussion about reconstruction can start immediately after diagnosis.
The decision to undergo breast reconstruction is an intensely personal one. The decision should be made by the patient, not by treating physicians. It really is a quality of life issue. And it doesn’t matter how old the patient is or if they’re married or single.
There are several surgical approaches to reconstructing a totally or partially missing breast. The choice of technique depends on age, health, the state of the remaining tissue, surgical scars, skin thickness, radiotherapy treatments, the shape and volume of the breast to be reconstructed and the remaining breast, etc.
Reconstruction may be simple, involving nothing more than the insertion of an implant, or more complex. In some cases, for instance, it may be necessary to replace local tissue with tissue from elsewhere in the body (a flap of skin or of skin and muscle). Step-by-step reconstruction is another option, for instance to adjust the size of the other breast, rebuild the nipple and so on.
Flap reconstruction is a more complex procedure than skin expansion. Scars will be left at both the tissue donor site and at the reconstructed site, and recovery time is longer than with an implant. However, when the breast is reconstructed with one’s own tissue, the results are generally more natural and concerns related to implants are non-existent.
Skin expansion
This common technique combines skin expansion and subsequent insertion of an implant. Following mastectomy, a balloon expander will be inseted beneath the skin and chest muscle. Through a tiny valve mechanism buried beneath the skin, he or she will periodically inject a salt-water solution to gradually fill the expander over several weeks or months. After the skin over the breast area has been sufficiently stretched, the expander is removed in a second operation and a more permanent implant — either saline or silicone — will be inserted. Some expanders are designed to be left in place as the final implant. The nipple and dark skin surrounding it — called the areola — are reconstructed in a subsequent procedure.
Flap reconstruction
An alternative approach to implant reconstruction involves creation of a skin flap using tissue taken from other parts of the body, such as the abdomen, back or buttocks. In one type of flap surgery, the tissue remains attached to its original site, retaining its blood supply. The flap, consisting of skin, fat and muscle with its blood supply, are tunneled beneath the skin to the chest, creating a pocket for an implant or, in some cases, creating the breast mound itself without need for an implant.
Another flap technique uses tissue that is surgically removed from the abdomen, thighs or buttocks and then transplanted to the chest by reconnecting the blood vessels to new ones in that region.
Recovery times for both procedures range from six months to one year, or longer, depending on individual circumstances.
Not all women are good candidates for breast reconstruction. Women who have had a mastectomy or Lumpectomy with radiation are typically not strong candidates for skin expansion reconstruction. Radiation changes the characteristics of skin tissue, causing a variety of complications ranging from excessive scar tissue development, to blood supply and overall healing problems. While radiation does present some difficult challenges, it doesn’t automatically rule out the possibility of reconstruction. While each circumstance is different, if there is enough good tissue to work with, reconstruction remains a viable option for most women.
Patients that are emotionally unstable should probably postpone reconstruction. Coping with the reality of breast cancer is an extremely overwhelming process. If a woman cannot understand the risks and limitations of reconstruction prior to her mastectomy surgery, I would recommend she wait.
Managing Misconceptions
Most misconceptions regarding breast cancer reconstructionare caused by a lack of information. Common misconceptions include having to wait up to one year to safely undergo reconstruction, reconstruction makes it difficult to identify cancer if it recurs, and reconstruction interferes with cancer treatments, such as chemotherapy. All are wrong on all counts.
Reconstruction can take place immediately following mastectomy with little complication. In the case of implants, reconstruction may take longer if the patient has to undergo chemotherapy, but otherwise doesn’t interfere with the process.
Managing Expectations
It is important to remember that the goal of reconstruction is improvement, not perfection. Be sure to discuss your expectations candidly with your plastic surgeon, and expect nothing less than total honesty from him or her in return. To ensure reconstructive surgery has the desired outcome, breast symmetry procedures – surgery to the other breast — is usually also part of the reconstructive process. Symmetry procedures either reduce, lift or reshape the remaining breast to ensure a better match to the reconstructed breast. Symmetry procedures can be an ongoing process, with periodic adjustments necessary to correct the affects of the aging process.
The information on this web site is only intended as an introduction to this procedure and should not be used to determine whether you will have the procedure performed nor as a guarantee of the result.
The best method of determining your personal options is to schedule a personal consultation with Dr. Makki. He will be able to answer specific questions related to your situation.
Please don’t hesitate to call for any questions that you might have
Breast Revision
Also known as breast implant replacement
Breast implant revision surgery, which commonly involves removal and/or replacement of saline or silicone gel implants, is performed to change the size or type of your implants and to correct any complications from your primary breast augmentation. The overall goal is to restore a youthful breast contour and appearance.
When to Consider Breast Revision
Your saline breast implants have deflated or an X-ray or MRI suggests your silicone implant has a shell leak
If you want to change your implant/breast size
If you have tightening of the scar tissue around the implant (capsular contracture) or your breast implants have shifted in position
If your breast tissue has changed as a result of skin stretching or weight loss/gain
Considerations
Pros
You will regain a youthful breast shape.
You may increase or decrease your breast size.
You will improve breast symmetry.
Cons
Gravity and aging will eventually alter the size and shape of your breasts.
The weight of your implants will also affect your breast appearance with time.
Your surgeon will need to have the surgical details of your first breast surgery.
These are the top three pros and cons to weigh when considering a breast augmentation revision. If you wish to focus on what is unique to you, please consult with one of our aesthetic plastic surgeons.
Are you a good candidate for breast revision?
Even if your breast implant surgery was perfectly planned and beautifully executed, changes can occur over time.
The following are some common reasons why you may want to consider revision surgery:
You are in good health.
You are not a smoker.
You wish to increase or decrease the size of your breasts.
You wish to correct breast asymmetry.
You want to address problems that have developed with your implants and/or surrounding breast tissue.
Pregnancy and/or breastfeeding has changed the appearance of your implants.
Weight loss or weight gain has negatively affected the appearance of your breasts.
You should have undergone a breast lift with your initial breast augmentation, but did not.
You are unhappy with the results of previous surgery due to poor implant placement or other aesthetic problems.
You wish to remove your breast implants permanently.
If you are in good general health, have a positive attitude and realistic expectations, you are most likely a good candidate for this procedure.
How is a breast revision procedure performed?
The exact procedure your surgeon will use for breast implant removal and replacement varies depending on the reason for your revision.
Change in breast size: If you decide to change your implant size, your surgeon will frequently use your original incision for implant removal and replacement. If you want a larger implant, your doctor will surgically enlarge the “pocket,” or space in the breast, surrounding your implant to accommodate a larger implant. If you want smaller implants, you doctor may surgically reduce the size of the pocket with sutures to properly fit smaller sized implants. A breast lift may be done at the same time.
Capsular contracture (hardening of the capsule and implant): Your doctor will probably use the same incision used to insert the original implants to remove the hardened capsule and implant. He or she will then insert a new implant.
Implant rippling: When the edges of saline implants are visible and palpable (able to be felt), your surgeon may use the same incision to remove or reposition the implants as was used to originally insert them. Other options include using a different type of implant or placing the new implant into a different breast pocket that either has thicker muscle coverage or uses other tissues to cover the implant edge.
Implant malposition: Sometimes implant pockets are created too far apart or too close together, resulting in poorly positioned breasts. To correct this, using the prior incision, your surgeon will manipulate the scar tissue from the capsule surrounding the implant and reconstruct the pocket in the appropriate position using suturing techniques. Your surgeon may need to utilize other tissues to reinforce this new implant pocket and may recommend using an acellular dermal matrix product. Known by the acronym ADM, Acellular Dermal Matrix eventually gets integrated into the body and is completely replaced by the patient’s own collagen resulting in a thicker, stronger layer of tissue than the one that would have developed in the absence of the ADM. It is natural and bioresorbable yet maintains its strength over time. ADM is attached with absorbable sutures to the existing capsule, anchoring it to its new position to add additional support.
Implant removal: If your implants are large and your skin has stretched, your surgeon may recommend a breast lift in addition to implant removal, but implant removal alone may suffice. The original incision created to insert the implant will almost always be the same one used to remove it. The lining around the implant, or “capsule,” is often surgically removed at the same time to facilitate rapid healing.
Elevation of nipple and areola position: If it is necessary to elevate the position of your nipples and areolas (pigmented skin surrounding the nipples), you will need additional incisions. Incisions around the upper portion of the areola will be adequate in cases where not much elevation is needed. When more lifting and tightening is necessary, an incision all the way around the areola, including a vertical scar extending down from the areola to the crease under the breast, may be necessary. For cases where significant excess skin needs to be removed (such as in women who have had massive weight loss), a third incision may be necessary that will extend horizontally beneath the breast, following the natural curve of the breast crease. If your nipples need lifting, the nipples and areolas remain attached to underlying mounds of tissue and this usually allows for the preservation of sensation and the ability to breastfeed.
The goal of your aesthetic plastic surgeon and the entire staff at PSC is to help you achieve the most beautiful and natural-looking results, as well as making your surgical experience as easy and comfortable as possible.
What are my options?
Good communication with your plastic surgeon is the key to achieving the results you want. It is your job to clearly state your aesthetic goals so your surgeon can suggest the right options. During your consultation, you and your surgeon will resolve these issues:
What type of implant will be used?
Silicone-filled breast implants are filled with soft, elastic silicone gel and are available in a variety of shapes. All silicone breast implants are prefilled and may require a longer incision for implant placement.
Cohesive gel silicone implants, also known as “gummy bear” or “form stable” implants, are filled with a cohesive gel, made of crosslinked molecules of silicone, which makes them a bit thicker and firmer than traditional silicone implants. This enables them to hold their shape better. Approved by the FDA for use in the United States in 2013, these implants have been available in much of the world since 1992.
Will your implant be located above or below the pectoralis major muscle?
Placement of the implant underneath the pectoral muscle (the muscle underlying your breast) may interfere less with mammograms and breastfeeding. Your surgeon will present the pros and cons of each option.
What will my breast revision incisions and scars be like?
The original incision used to insert the implant is almost always the same one used to remove it; however, if you undergo a breast lift, elevating the position of your nipple and areola will result in breast lift scars (see How is breast revision performed?).
Your initial consultation appointment
During your initial consultation, you will have the opportunity to discuss your cosmetic goals. Your surgeon will evaluate you as a candidate for breast revision and clarify what a breast revision can do for you. Once your surgeon understands your goals and medical condition, both alternative and additional treatments may be considered (see related procedures).
Your plastic surgeon will examine, measure and photograph your breasts for your medical record. Your surgeon will consider:
The current size and shape of your breasts.
What kind of implant you currently have.
The breast size and shape that you desire.
The quality and quantity of your breast tissue.
The quality of your skin.
The placement of your nipples and areolas.
If your breasts are sagging, a breast lift may be recommended in conjunction with breast implant revision.
You should come to the consultation prepared to discuss your complete medical history. This will include information about:
Past and present medical conditions
Allergies and current medication
Medical treatments you have received
Previous surgeries, including breast biopsies
Family history of breast cancer
Current mammogram results
If you are planning to lose a significant amount of weight, be sure to tell your plastic surgeon. The surgeon may recommend that you stabilize your weight before undergoing surgery.
If you think that you may want to become pregnant in the future, discuss this with your surgeon. Pregnancy can alter breast size in an unpredictable way and could affect the long-term results of your breast revision.
Your treatment plan
Based on your goals, physical characteristics, and the surgeon’s training and experience, your surgeon will share recommendations and information with you, including:
An approach to your surgery, including the type of procedure or combination of procedures.
The outcomes that you can anticipate.
Your financial investment in the procedure.
Associated risks and complications.
Options for anesthesia and surgery location.
What you need to prepare for your surgery.
What you can expect to experience after surgery.
Show before-and-after photos of cases similar to yours and answer any questions.
Questions to ask your aesthetic plastic surgeon
It is important for you to take an active role in your surgery, so please use this list of questions as a starting point for your initial consultation.
Am I a good candidate for a breast revision?
Are the results I am seeking reasonable and realistic?
Do you have before-and-after photos I can look at for the procedure I am undergoing?
Will my scars be visible? Where will my scars be located?
What kind of anesthesia do you recommend for me?
What will be the costs associated with my surgery?
What will you expect of me to get the best results?
What kind of recovery period can I expect and when can I resume normal activities?
What are the risks and complications associated with my procedure?
How are complications handled?
What are my options if the cosmetic outcome of my surgery does not meet the goals we agreed on?
How do I prepare for a breast revision procedure?
Your surgeon will provide thorough pre-operative instructions, answer any questions you may have, take a detailed medical history and perform a physical exam to determine your fitness for surgery. In some instances, you may need to have a mammogram before revision surgery.
In advance of your procedure, your surgeon will ask you to:
Avoid taking aspirin, certain anti-inflammatory drugs and some herbal medications that can cause increased bleeding.
Stop smoking at least six weeks before undergoing surgery to promote better healing.
Regardless of the type of surgery to be performed, hydration is very important before and after surgery for safe recovery.
If your surgery is to be performed on an outpatient basis, be sure to arrange for someone to drive you home after surgery and stay with you for the first day or two, unless you and your surgeon have decided on other post-operative recovery options.
Before surgery, stock your refrigerator with high-protein, low-sodium foods, including premade meals, fresh fruits and vegetables, and lots of caffeine-free beverages and water. Avoid food and drink containing salt during your recovery.
As you heal, your arms will have a limited range of motion, so store all the supplies you’ll need during recovery where they’re easily accessible (at counter level, not in overhead or very low cabinets).
Establish a no-fail support system for the full recovery period indicated by your surgeon. This is critical to your recovery. If you have children less than five years of age, you must have someone to take care of them for a week. You must not lift, drive, or do laundry and cleaning for the first two weeks.
Rest and sleep on your back continuously in an inclined position (25- to 45-degree angle) for the initial post-operative days or while significant swelling remains. You can achieve elevation with wedge pillows with an incline design or by sleeping in a recliner chair.
Avoid hot showers, hot tubs and saunas for two to three weeks.
Decide what you will wear for the first few days; pick items that open in front. Wear slip-on shoes so you don’t have to bend.
Breast revision is usually performed on an outpatient basis. Be sure to arrange for someone to drive you home after surgery and to stay with you at least the first night following surgery.
What can I expect on the day of revision surgery?
Your revision surgery may be performed in a hospital, free-standing ambulatory facility or office-based surgical suite. Your surgeon will give you an estimate of how long your surgery will last based on the details of your surgical plan.
You may be asked to wash your body with antibacterial soap prior to surgery.
Make sure not to wear makeup (including nail polish), lotions, perfumes or other substances.
Dress in or bring soft, comfortable clothes that you’ll be able to wear after the surgery, including a top that opens in the front and shoes that slip on.
Bring only the essentials (ID, cell phone, etc.) and leave other personal belongings such as jewelry at home.
Medications are administered for your comfort during the surgical procedure.
General anesthesia is commonly used during your revision procedure, although local anesthesia or intravenous sedation may be desirable in some instances.
For your safety during the surgery, various monitors will be used to check your heart, blood pressure, pulse and the amount of oxygen circulating in your blood.
Your plastic surgeon will follow the surgical plan discussed with you before surgery.
Once the operation has begun, the surgeon may decide to combine various techniques or change a technique to ensure the best result. It is important that you feel comfortable and trust your doctor to make these decisions.
Following the surgery, a bulky gauze dressing (bandage) will be wrapped around your breasts and chest, or you might wear a surgical bra. Drainage tubes may be attached to your breasts.
After your surgery is completed, you will be taken into a recovery area, where you will continue to be closely monitored.
When you are fully alert, you will be able to go home with the assistance of a friend or family member. Before leaving for home, you (or someone looking after you) should feel capable of emptying and resetting the drains.
You will probably be permitted to go home after a short observation period unless you and your plastic surgeon have made other plans for your immediate post-op recovery.
Aftercare and Recovery
Your surgeon will discuss how long it will be before you can return to your normal level of activity and work. After surgery, you and your caregiver will receive detailed instructions about your post-surgery care, including information about:
Drains, if they have been placed
Normal symptoms you will experience
Potential signs of complication
Immediately after your breast revision surgery
Your post-operative discomfort and recovery time will be similar to that of your primary breast augmentation. You should be up and walking on the day of surgery. It will take several days to return to more normal activities after your breast implant revision, but it is important to your recovery that you get up and move around. The extent and duration of discomfort depends largely on the size and placement of the implants, and may include pain, stiffness, swelling, bruising and itching.
When the anesthesia wears off, you may have some pain. If the pain is extreme or long-lasting, contact your physician. You will also have some redness and swelling after the surgery. Contact your surgeon to find out if your pain, redness and swelling are normal or are signs of a problem.
Recovery time frame after breast revision
It is vitally important that you follow all patient care instructions provided by your surgeon. This will include information about wearing compression garments, care of your drains, taking an antibiotic, if prescribed, and the level and type of activity that is safe. Your surgeon will also provide detailed instructions about the normal symptoms you will experience and any potential signs of complications. It is important to realize that the amount of time it takes for recovery varies greatly among individuals.
Undergoing a breast lift in conjunction with breast implant removal will lengthen your recovery time. If your breast implants are removed entirely, your recovery will likely be brief, with minimal discomfort. Avoid heavy physical activity for at least the first two weeks following surgery. After that, be gentle with your breasts for at least the next month. Your plastic surgeon will give you specific instructions and restrictions about physical activity.
The first week
For the next week, you will benefit from sleeping with your head and back elevated to reduce swelling in the chest area. You can use pillows, a wedge pillow, or sleep in a recliner chair.
Your plastic surgeon will probably permit you to shower one to three days following surgery, but do not immerse your breasts in a tub, spa or Jacuzzi for at least four weeks after surgery.
Depending on your plastic surgeon’s preference, your dressings will be removed within a few days after surgery.
If drains are placed, don’t shower until 24 hours after the drains are removed, which is usually after three days.
You may be instructed to wear a compression bra during your early healing period to prevent fluid accumulation, control swelling and keep implants in place during the initial healing period.
Stitches that don’t dissolve on their own will be removed in about a week.
Some discoloration and swelling may occur initially, but this will resolve as you heal.
Two to six weeks
Most residual swelling will resolve within a month.
After breast revision surgery, it is often possible to return to work within seven to ten days, depending on the type of activities you perform.
If you selected large implants, the skin around the breasts may feel tight as your body adjusts to accommodate the size increase.
Long term
It may take several weeks or months for new implants to “settle” into their final position. Altered sensation, such as numbness or tingling, may be present around the incision site, but this should decrease over the following weeks or months.
How Long Will the Results Last?
Unless you gain or lose a significant amount of weight or become pregnant, your new breast shape should remain fairly stable. However, gravity and the effects of aging eventually alter breast size. The weight of the implant used will also affect how your breasts appear as time goes on. Breast implant revision results are long-lasting; however, you may want to periodically visit your doctor to help prevent any further complications.
Maintain a relationship with your aesthetic plastic surgeon
For safety, as well as the most beautiful and healthy outcome, it’s important to return to your plastic surgeon’s office for follow-up evaluation at prescribed times and whenever you notice any changes. Do not hesitate to contact your surgeon when you have any questions or concerns.
Limitations and Risks
Fortunately, significant complications from breast revision surgery are infrequent. Every year thousands of women undergo successful breast revision surgery and are pleased with the results. This surgery is usually performed without any major problems. Your specific risks for breast revision will be discussed during your consultation.
All surgical procedures have some degree of risk. Some of the potential complications of all surgeries are:
Adverse reaction to anesthesia
Hematoma or seroma (an accumulation of blood or fluid under the skin that may
require removal)
Infection and bleeding
Changes in sensation
Scarring
Allergic reactions
Damage to underlying structures
Unsatisfactory results that may necessitate additional procedures
You can help minimize certain risks by following the advice and instructions of your board-certified plastic surgeon, both before and after your breast revision surgery.

 Twitter
Twitter Facebook
Facebook Instagram
Instagram Google +
Google +